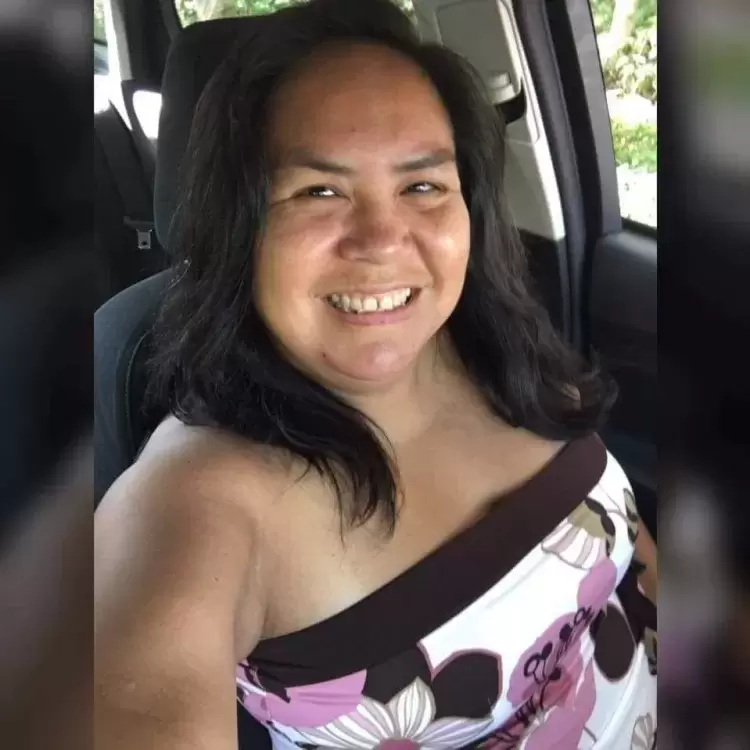
Vanessa Sim, a Hesquiaht woman, wasn’t feeling well and decided to get checked at West Coast General Hospital on June 18.
“I was endlessly thirsty, needed the bathroom a lot and was feeling confused,” said Sim, a wife, mother and grandmother. She said her family was concerned because she would blurt out random things, not seeming to make sense. On top of that, her vision was going bad.
Concerned about her worsening symptoms, Sim went to visit the emergency department at West Coast General Hospital to get checked out.
She sat in triage for four hours before hospital staff asked if she had a blood test. She hadn’t been tested but answers came quickly once the results came back.
“You have diabetes,” the doctor blurted from the foot of the bed. There was no sugar coating it. Sim was left to process her new reality of being a Type 2 diabetic.
According to Diabetes Canada, Type 2 diabetes is a disease in which your body cannot make enough insulin (a hormone that helps control the amount of glucose, or sugar, in your blood) or does not properly use the insulin it makes.
According to the Canadian Journal of Diabetes, Indigenous people around the world are at higher risk for developing diabetes.
“The higher rate of adverse health outcomes in Aboriginal peoples is associated with a number of factors, including lifestyle (diet and physical activity), genetic susceptibility, and historic-political and psychosocial factors, stemming from a history of colonization that severely undermined Aboriginal values, culture, and spiritual practices,” wrote the journal.
In other words, our ancestors were more physically active and ate a healthier diet of seafoods, land mammals, roots, and berries.
“People over the age of 40 with a parent or sibling with diabetes are at a higher risk of having Type 2 diabetes,” says Diabetes Canada.
Sim says her late father and her brother were both diagnosed with Type 2 diabetes. But she didn’t recognize the signs. She only knew something was wrong with her body.
“I craved orange juice and yogurt drinks,” she told Ha-Shilth-Sa. She drank a lot of water to try to relieve her unquenchable thirst.
“Drinking too much water dilutes your sodium levels,” she said, adding that this is what brought on confusion.
Sim had already started to make healthier food choices prior to her trip to emergency. She stopped taking sugar in her coffee and began eating more salads.
Once she started treatment for her condition, she said it was like doing a 180 – things got better quickly. In the five weeks since her diagnosis she dropped 30 pounds.
“I stopped having sugary drinks,” she said, adding that she mostly misses her red raspberry slushies from the convenience store. She also spends a lot of time reading food labels to avoid high sugar or carbohydrate foods.
Sim began taking prescribed Metformin and spent 90 minutes with a dietician, who taught her what foods she can and can’t eat, and about portion control.
“I can have as much veggies as I can,” she said, adding that she’s discovered that she loves hummus as a dip, rather than the commercial dairy dips and sugary salad dressings.
She must monitor her sugar levels everyday with finger pokes to test her blood and she goes to the hospital lab every month for blood tests.
“I’m sleeping better, my skin has improved and my vision…I don’t need to wear glasses for driving anymore,” she said. Sim also noticed that her stress levels have gone down.
Prior to her diagnosis, Sim said her family ate a lot of take-out food but now she must change what she eats.
“Sometimes I really want something I shouldn’t have, but I’ll just have my veggie sticks and hummus and my body feels so much better for doing that,” she said.
Sim advises people to get to know their bodies and if something feels off, go get checked.
According to Diabetes Canada, the disease affects one in three Canadians. Diabetes can be managed with healthy food, regular exercise, and in most cases, medication.
They go on to say a good first step is to cut out highly processed foods, refined grains such as white bread, sugary food, and sugary drinks. Instead, plan your meals around vegetables, plant-based proteins, whole grains, dairy, lean meats, oily fish, nuts, and healthy oils such as olive oil. And remember to keep moving by going for walks or other regular exercise.