Spring is in the air and so is pollen. For seasonal allergy sufferers, that means a trip to the pharmacy for costly antihistamines. What many Aboriginal people don't know is that these types of medications are covered under the BC PharmaCare Plan W program and can be accessed free of charge.
The BC PharmaCare Plan W covers eligible First Nations and Inuit people in the province. You are eligible for coverage under the Plan W if you have active Medical Services Plan (MSP) coverage, and are a registered Indian under the Indian Act. Children under one year old that have at least one parent registered under the Indian Act are also eligible.
Members of treaty nations should check with their administration office for information about health coverage provisions under their treaty.
Prior to October 2017, medical services and supplies were administered through the federal Non-Insured Health Benefits (NIHB) Program. This covered prescription drugs, over-the-counter medication, medical supplies and equipment, mental health counselling, dental care, vision care, and medical transportation to eligible First Nations and Inuit.
On October 1, 2017, First Nations Health Authority (FNHA) clients joined the BC PharmaCare program, taking over delivery of medical benefits to eligible clients who had been receiving benefits through Health Canada's Non-Insured Health Benefits (NIHB) program.
Today, the BC PharmaCare program delivers similar health benefits to First Nations people under Plan W. Funded by FNHA, Plan W covers 100 percent of eligible prescription costs and certain medical supplies, various over-the-counter drugs, some natural health products, and pharmacy services; it covers most OTC (over the counter) medications previously covered by NIHB, under similar rules.
There is a list of medications called the Plan W Formulary; it is a listing of medications and supplies that are covered under Plan W and can be found on the FNHA and the BC Ministry of Health websites.
Included on the list are OTC products deemed appropriate for pharmacist-initiated treatment, meaning you don't need to get a prescription from your doctor. The pharmacist can dispense certain OTC medications, billing the Plan W program directly.
Medication for allergy sufferers is included on the list OTC products that don't require a doctor's prescription.
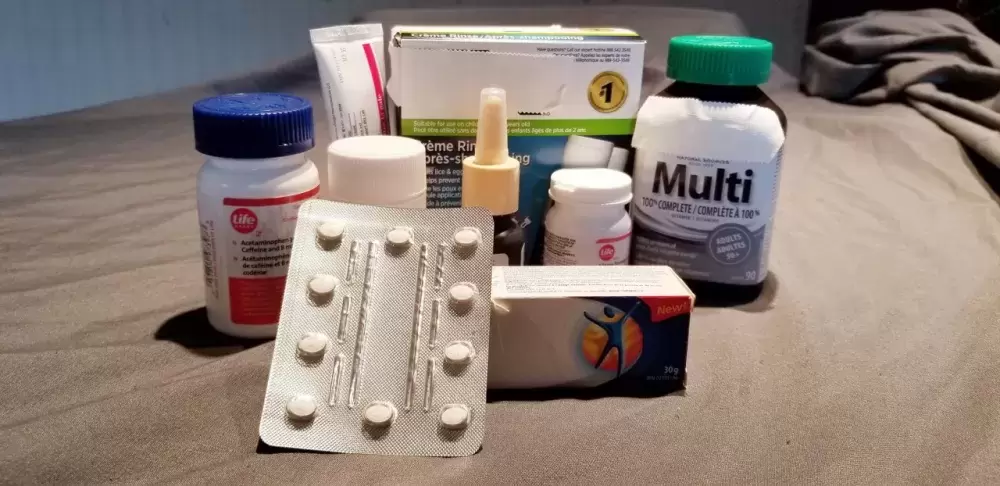
Other items on the list are certain treatments for eye, nasal and oral medication for allergy sufferers, treatments for acne, diabetes supplies, lice treatment, emergency contraception, topical antibiotic ointment for skin/eyes, products to treat constipation, anti-fungal skin cream, prenatal vitamins and vitamins for children.
To get your OTC medication covered under your plan you need to call or visit your pharmacist ahead of time. They will advise you if it is necessary to get a doctor's prescription for your OTC medication. If a prescription is not necessary, the pharmacist will take your Care Card number for billing purposes then prepare your OTC medication.
There is a 17 page list of approved OTC medications for Plan W clients that can be found online at https://www2.gov.bc.ca/assets/gov/health/health-drug-coverage/pharmacare/planw-otc-meds.pdf
The list includes pain relievers like acetaminophen (Tylenol), ASA (Aspirin) and ibuprofen (Motrin). Also on the list are medications to treat nausea/vomiting, lactose intolerance, warts, diaper rash as well as a variety of vitamin and mineral supplements.
Information about Plan W can be found on the BC Ministry of Health website.
The list of approved pharmacist-initiated OTC medications is here: https://www2.gov.bc.ca/assets/gov/health/health-drug-coverage/pharmacare/pharm_initiated_otc.pdf