On April 1 the province set out to provide free contraception to all British Columbians covered under MSP.
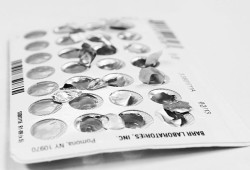
This includes oral contraceptives, intrauterine devices (copper and hormonal), hormonal implant, hormonal injection, and emergency contraception, such as Plan B, which requires no prescription.
The First Nations Health Authority will continue to fund patches and rings, which are not included in recent changes, said Dr. Unjali Malhotra, the FNHA’s medical director, who specializes in women’s health.
“There shouldn't be any issues surrounding coverage for any First Nations person that is registered with the First Nation Health Authority,” said Malhotra. “It's very exciting that we have free contraception in British Columbia… and what's even more exciting is we can have a conversation surrounding access.”
In September 2022 it was announced that the Ministry of Health and the College of Pharmacists of B.C. would develop regulations to allow pharmacists to prescribe medication for minor ailments and contraception.
It was recently announced that this would begin on June 1. With this change individuals seeking a contraceptive prescription or counseling can receive these services at a pharmacy.
Malhotra explains that having pharmacists provide contraceptive counseling and prescribing will reduce barriers that people have, especially those living remotely.
“Reducing the number of contact points for some people is a really good thing,” said Malhotra.
Additionally, in September of 2022 the BC College of Nurses and Midwives approved a new scope of practice for registered nurses who are certified to prescribe. The Ministry of Health continues to work with institutions on training requirements, while RNs are currently not authorized to prescribe contraception.
“The college sees that we need to expand our practice in order to help with the doctor shortage,” said Lucy Chiasson, a community health nurse at the Strong Family House, when reflecting on expanded roles for pharmacists and nurses. “I think that's probably part of the reason why that's being expanded.”
Malhotra goes on to explain that, though it is currently pending as to when a certified RN can prescribe contraception, the FNHA is in favor of broadening their scope of practice.
“The increase in numbers of folks that have the opportunity to offer prescriptions and counseling is a really important movement forward,” said Malhotra. “What we want to see is an increase in access and a reduction in barriers in all circumstances.”
Kelsey Rix (Hahahtmaq aqsa), a community health nurse in Ahousaht, said that she would like to be able to have contraception in her community to give to members who require it. She would also like to see emergency contraception on hand in communities so that nurses can dispense it.
“I still need a doctor's prescription to be able to give people birth control,” said Rix. “I can educate them and I can discuss everything with them while they're in my office, but it's been a barrier to go to the doctor to get the prescription.”
For those located in Ahousaht, a remote community on Flores Island near Tofino, they have to take a boat off the island to the closest pharmacy or clinic in places such as Tofino, Ucluelet, or Port Alberni to receive a doctor’s prescription or contraception, including emergency contraception, explains Rix.
Rix explains that youth are among those who are likely to not seek out contraceptive care, so it’s important to meet them where they are at.
She explains that in Ahousaht, twice a week there's a doctor on site, but for the youth a barrier is confidentiality due to the close-knit community. Youth also might not be able to afford taking a boat to Tofino to obtain pharmacy items like emergency contraceptives, she continued.
“We want to meet them where they're at, in that moment, because we just don't know what else is going on in their life that's already been a barrier for them to come and ask us in the first place,” said Rix.
According to the PharmaCare Newsletter from March 8, 2023, with the recent changes people can request multiple doses of emergency contraception and a larger supply of oral contraception. Health providers warn against using emergency contraception as a regular form of birth control.
Chiasson said these changes create “less barriers” for those living in remote communities.
But Malhotra noted that, beyond financial barriers, logistical and geographical challenges to getting birth control also need to be considered.
“No one piece of this is going to create a perfect situation,” said Malhotra. “However, a combination of change will lead to significant improvement to access.”
“We continue to work with our trusted partners on decreasing geographical barriers because we want to ensure they have access to culturally safe care as close to home as possible,” she added. “These are important steps in making that happen.”
Malhotra explains that having access to culturally safe care means receiving medical help that is respectful, engaging, and safe. This means that it is free of discrimination, racism, and bias, she continued.
“We have to realize that many of the community members are living in rural and remote areas,” said Chiasson. “Having that ability to have access to birth control means that they're in control.”