A joint report released Thursday by the First Nations Health Authority and BC Cancer Agency has spelled out some of the disparities in cancer rates and survival rates between Indigenous and non-Indigenous Peoples in B.C.
In short, it’s a good news/bad news situation. Despite a perception that cancer rates are at epidemic levels in First Nations communities, cancer rates are actually somewhat lower than in non-Indigenous communities. But First Nations members are less likely to receive timely cancer diagnosis and intervention, leading to higher death rates (that is in 10 of the 15 cancer types examined in women and 10 of the 12 cancer types examined in men).
Following the news conference, Ha-Shilth-Sa spoke with two B.C. Cancer Agency spokespersons, Dr. John Spinelli, Vice President of Population Oncology, and Preston Guno, Director of Indigenous Care.
Spinelli said the lower-than-expected cancer incidence rates were encouraging.
“But the fact that survival rate is lower is of concern,” Spinelli said, noting that the study did not break down rates between urban, rural and remote populations. “But the survival was pretty consistent – lower in almost every type of cancer.”
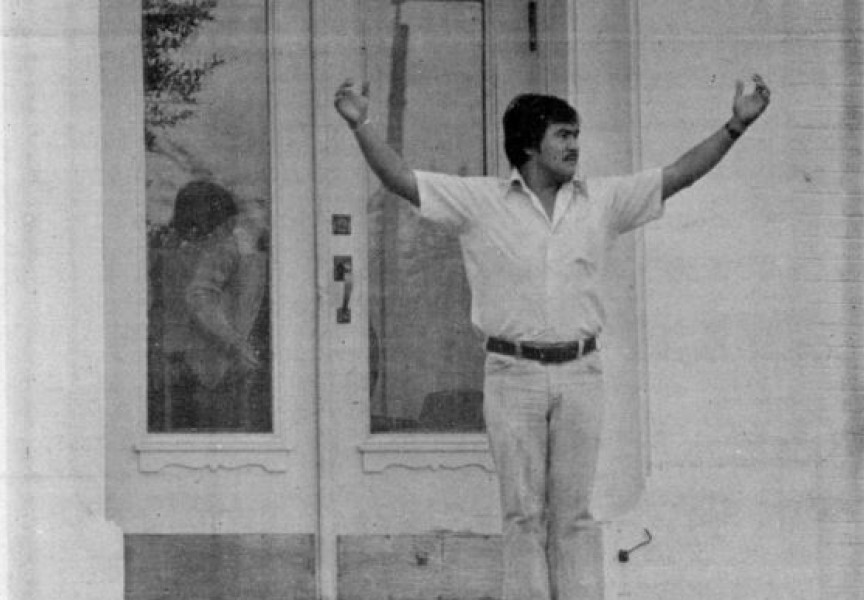
Guno, a member of the Nisga’a Nation, said the study also reflects the lingering social effects of colonialism, and more specifically, the residential school system, on how First Nations people perceive and deal with the health care system. The goal is to improve that relationship, in partnership with the First Nations Health Authority.
“We know that wellness [programs], prevention, screening and distance care can all be improved on,” he said. “We need to work together to improve access to care.”
Guno said the innovative TeleHealth program, which allows patients to consult with physicians by telephone, is one way to improve access to health care for people in remote communities. But much more support is needed, he said.
The study was jointly conducted between 1993 and 2010, by the B.C. Cancer Agency and the First Nations Health Authority, and can be accessed in full on the Cancer Causes & Control website at https://link.springer.com/article/10.1007/s10552-017-0950-7.
Despite the generally similar cancer incidence rates, First Nations men and women experience a significantly higher rate of colorectal cancer than their non-Aboriginal neighbours – 22 per cent higher for women and 39 per cent higher for men.
Spinelli said the reason for the disparity is not fully understood, but BCCA has already taken steps to address it.
“We have created a provincial colorectal screening program, but the program was only set up in 2013, after the study was completed,” he said.
The screening technology is capable of detecting pre-cancerous tissues, Spinelli explained. When detected early, colorectal cancer can be treated effectively and less invasively. The challenge is to encourage First Nations people to seek out and undergo screening. Part of that is simply letting people know it is available.
The disparity in rates for cervical cancer is disturbing – First Nations women are 92 per cent more likely to contract cervical cancer than non-Aboriginal women.
“That’s another area where we can make improvements,” Spinelli said. Early vaccination for the HPV virus, which has been linked to cervical cancer, can drastically lower cancer rates, he explained. Early screening and testing improve detection and diagnosis, raising survival rates for those who go on to contract the disease.
Again, the goal is to encourage more First Nations women to overcome any reluctance to engage with the health care community.
“What really resonates with this study is the need for a more culturally-sensitive approach,” Guno said. It is well established that First Nations people are more likely to access care that respects their wellness beliefs and goals.
The incidence of lung cancer is a picture that is currently evolving and not in a positive direction. While lung cancer rates are generally lower for First Nations people, the incidence is rising, while at the same time, rates for non-aboriginal people are declining. At some point in the near future, the incidence of lung cancer among First Nations people is expected to exceed that of the non-aboriginal population.
Spinelli said the goal now is to expand the collaboration between BCCA, the FNHA and all health authorities within the province, and to continue collecting First Nations cancer data.
“This is really only the first step,” he said.
In a post-conference news release, FNHA Chief Executive Officer Joe Gallagher set out an ambitious set of goals to improve the health prospects for B.C. First Nations.
“Our systems-wide response to improve the First Nations cancer journey must include working with communities to help prevent cancer before it starts; increasing access to colon, cervical and breast cancer screening; promoting cultural safety and humility in cancer care services; supporting First Nations cancer survivorship and end-of-life journeys; improving knowledge on the First Nations cancer journey; and nurturing partnerships between First Nations communities, the FNHA, and health system partners.”
The FNHA, BCCA, the B.C. Association of Aboriginal Friendship Centres and Métis Nation are working in partnership to complete an Indigenous Cancer Strategy to be released later this fall.