The province is imposing an overbearingly institutional system on B.C.’s young people who struggle with mental health issues, thereby failing those who need the support the most, according to a recent report from the Representative for Children and Youth.
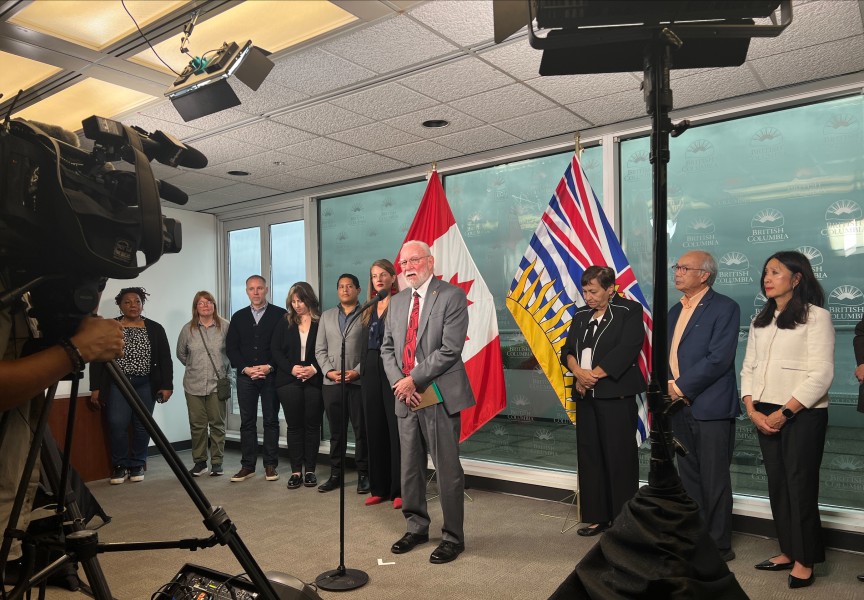
On Tuesday Jennifer Charlesworth released a critical study of how the B.C. Ministry of Mental Health and Addictions is serving vulnerable young people in the province, noting that forced detentions into treatment facilities has gone up 162 per cent over a decade.
That statistic covers the period from 2008-2018, showing a rising number of involuntary detentions undertaken according to provisions of the Mental Health Act. According to the provincial legislation, a young person can be kept against their will if they present a safety risk to themselves or others - or if this is deemed necessary to prevent “mental or physical deterioration”. The act allows treatment to be imposed on those who are detained, as well as discipline, restraint and isolation, states the representative’s report.
But much more can be done to ensure young people’s rights are upheld, argues Charlesworth, who challenges the value of how youth are treated while detained.
“I am concerned that a standout memory for many young people is being isolated and restrained,” she said in a press release. “The absence of legislation and regulation to guide the use of this extraordinary power is also troubling. The fact that these measures are coercive and may be experienced as traumatizing underlines the need for rigorous oversight and accountability.”
Charlesworth’s report drew from interviews with youth, more than half of whom disagreed with their treatment for mental health issues.
“I’d wake up…and either be calm and go back to sleep or freak out and get sedated again,” said Sean, whose comments are included in the document. “It was like that for about three months. It’s just a big blur.”
“They said I could call a lawyer. I don’t have one and I hate court. I just waited it out,” noted Charlie, another young man who was interviewed. “I was an eagle trapped in a cage. I can’t fly or enjoy things. They took that away from me.”
Charlesworth noted a serious lack of community supports that are available for young people upon discharge, and recommends better oversight of detentions, with the involvement of independent bodies that advocate for patients.
Little data is available on the involuntary placements in facilities, but the Ministry of Health believes that Indigenous youth are disproportionally represented. Charlesworth stressed that a young person should be able to notify their First Nation if detained, and points to the absence of cultural relevant treatment for Aboriginal kids.
“The bottom line is that the Mental Health Act was not designed with the needs of children and youth in mind and is not meeting the needs of young people in this province,” she said. “Generally, they were looking for therapeutic support but found that, instead of that, what they received was forced medication.”
Back in the summer an amendment to the Mental Health Act was tabled in Victoria, which some feared would put Aboriginal youth at an even greater risk by expanding the use of detention.
“It wasn’t addressing the issue that youth find themselves in,” said Judith Sayers, president of the Nuu-chah-nulth Tribal Council. “Just throwing them in to be assessed for seven days doesn’t address the problem.”
The Union of BC Indian Chiefs opposed Bill 22, warning that it would lead to more fatal drug overdoses.
“Our families and communities require culturally safe, wraparound services – not additional legal mechanisms to detain our youth and ignore our rights,” stated Kukpi7 Judy Wilson of the UBCIC in July.
With the NDP still without a majority of seat in the legislature, Bill 22 did not pass last summer. But the need remains to change the provincial law to better serve vulnerable people, added Sayers.
“If they’re going to be amending the Mental Health Act, we can’t just put them in an institution because we know it doesn’t work,” she said. “They really do need to amend the Mental Health Act so this doesn’t happen, but at the same time we need to have something alternatively for them to utilize.”
Charlesworth’s report largely drew on information from before COVID-19 transformed the delivery of health services in the province. Since the pandemic began in March, youth have faced a growing list of challenges in maintaining mental health. Initiatives like the Warriors Program, which fosters a sense of brotherhood while building leadership qualities through land-based learning, have been affected by the inability to gather. Since March the six Nuu-chah-nulth nations that run the program have been unable to hold weekly meetings or camping excursions.
Teechuktl Mental Health has had to adapt to the elevated risk by closely monitoring social media posts to catch warning signs of self harm.
In response to Charlesworth’s report, Sheila Malcolmson, B.C.’s minister of Mental Health and Addictions, committed to listening to young people and their families.
“Our main focus continues to be on boosting the voluntary system of care so young people can get help early on, before smaller problems become larger ones,” she said in a statement.
Meanwhile, Malcolmson pointed to how mental health services have improved since her ministry was formed nearly four years ago.
“We’ve been making progress for young people in B.C. since 2017 by expanding voluntary services that support them,” she said. “New Foundry centres, child and youth teams in school districts, doubling the number of youth substance use treatment beds and expanding specialized services are just some of the examples.”