Nuu-chah-nulth Tribal Council nurses are working hard to continue patient care during a time of social isolation. By the very nature of the job, patient care is an intimate, hands-on service usually requiring face-to-face visits. Now, amid a pandemic, personal visits between nurses and their clients have been scaled back dramatically.
“Things have changed majorly,” said Homecare Nurse Clinical Leader Catherine Gislason, adding that normally nurses are out in communities, meeting with people, and checking on their service plans. “We have to be a lot more careful when we’re out with people making sure it’s safe for the nurses and for the clients.”
The nurses must weigh risks and benefits of the services that they can and can’t deliver. For example, they are not providing footcare during the pandemic.
“There is no person-to-person contact other than the few that must be seen and can’t be put off,” said Gislason, adding that when they must see a client they have to be COVID-safe about it.
According to Gislason, the 18 NTC nurses that deliver homecare services have adjusted in a way that ensures safety for both the patient and the nurse.
“During COVID-19 we are doing mostly everything by phone,” said Gislason.
She noted that six of the NTC homecare nurses have dual duties, spending some of their time working as community care nurses.
Homecare nursing allows clients with healthcare needs to be seen at home rather than having to stay in a health-care facility.
“We make sure they have everything they need and are looked after,” Gislason said.
In some cases, such as dressing changes, injections and checking in with palliative care patients, face-to-face visits are required.
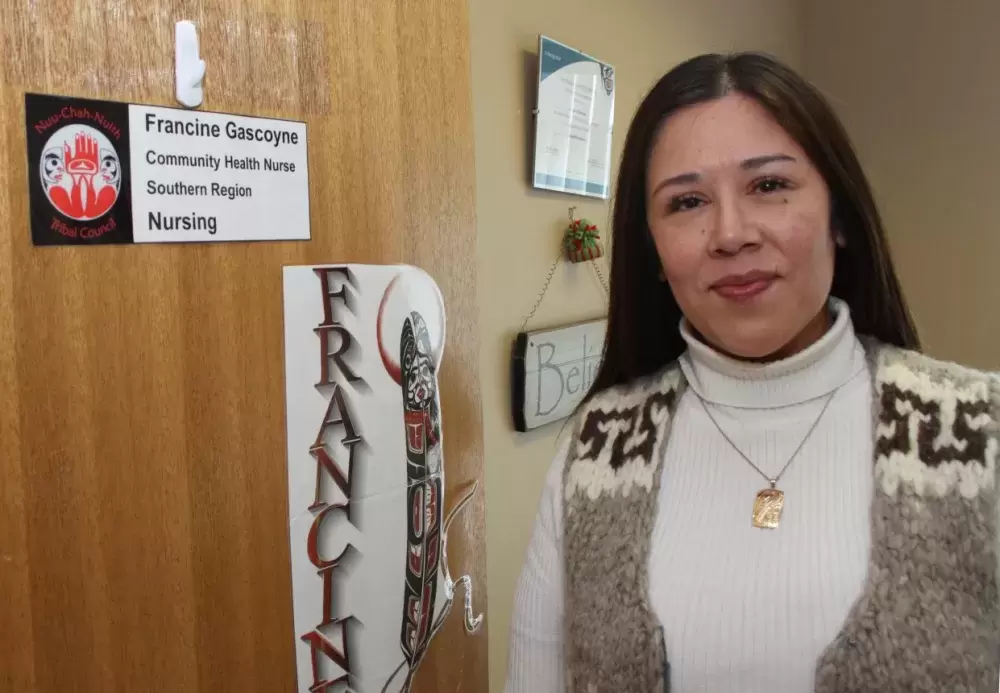
Francine Gascoyne, who is also a community health nurse clinical leader with the NTC, says that the nursing staff continue to deliver essential services to the communities. In keeping with social distancing requirements, Gascoyne has been busy, working from home, connecting with other health professionals by phone, email and teleconferencing.
Nursing without personal contact
Service delivery to remote communities has had to change. Gascoyne says during the pandemic, in-person nursing services to Nitinaht Lake, Anacla, Hot Springs Cove, Kyuquot, Zeballos and Tsaxana have stopped. However, the nurses do telephone check-ins with clients and keep in close contact with health leadership within the communities, providing support to them.
“Nurses always travel to the remote communities in pairs for safety and you can’t keep six feet apart in a vehicle,” said Gislason.
In addition, community leaders are working hard to keep their communities safe by limiting visits from outsiders.
“They are doing their best to keep their communities safe and we recognize that,” said Gislason, adding that the more people move around the more risk there is.
With that in mind, she said that the nurses that must travel to communities to deliver essential services like immunizations now perform these tasks at community health centres, not in private homes.
“We slowly started rolling out community health nurse essential services,” Gascoyne said.
Immunization clinics must resume
Careful to limit personal contact, NTC nurses will begin going back into the communities, starting with Ahousaht, Tseshaht, Ty-Histanis and a family clinic in Port Alberni, doing things like routine immunization clinic for babies and children.
“The provincial health officer encourages us to provide this essential service (immunizations) because we don’t want to another type of epidemic,” said Gascoyne.
Since the March 20 office shut down, the NTC nurses are checking in with patients by telephone.
Some nurses are still providing pregnancy tests, STI (sexually transmitted infection) screening, and are offering harm reduction supplies like naloxone kits.
“The opioid crisis is still a public health emergency,” said Gascoyne.
In addition, the nurses stay connected with prenatal and postnatal clients.
“Some nurses use Zoom to connect, and can see babies through this application,” said Gascoyne.
“We look after a lot of people so it’s a lot of phone calls, a lot of checking in and we’re keeping in touch with each of the communities as well,” Gislason said.
NTC homecare nurses will, in some cases, check in daily with high priority people, such as those in fragile health situations.
“Everyone is getting what they need; we’re doing the urgent care that we need to and keeping in contact with rest by phone, Zoom, video calling, texting and social media, whatever is available,” said Gislason.
The NTC’s Aboriginal liaison nurse provides services to Nuu-chah-nulth people at the hospital. She normally works at the West Coast General in Port Alberni, but is also working from home during the pandemic.
“She is aware of who is entering and being discharged from the hospital and is working on meeting their needs at home,” said Gislason. “We’re working on getting her back into the hospital.”
Lesley Cerney, the NTC’s nurse navigator, delivers services to Nuu-chah-nulth people living away from home. “She is like the NTC Aboriginal liaison but outside the hospital,” said Gislason.
Expanded testing for COVID-19
While there is no definite end in sight to social restrictions, the NTC nurses are looking forward to getting back to normal duties in the not too distant future. “We are learning more about the virus and how to be more safe,” said Gislason. “We will be looking at how to safely get back to work when the time comes.”
What they do know is that the virus is still out there, and people are still getting sick.
“It’s out there, but if we are vigilant, stay home and stay away from one another it will eventually die off,” said Gislason.
Gascoyne said that the province has expanded its COVID-19 testing strategy. Before late April this testing was limited to only those with sever symptoms, health care workers and nursing home residents.
“It now includes anyone with cold, influenza or COVID-19-like symptoms, however mild,” said Gascoyne.
While testing has expanded, not everyone needs a test. COVID-19 testing is not recommended for people without symptoms.
The symptoms of COVID-19 are similar to other respiratory illnesses, including the flu and common cold. They include: fever, chills, cough, shortness of breath, sore throat, painful swallowing, stuffy or runny nose, loss of sense of smell, headache, muscle aches, fatigue, and loss of appetite.
Any doctor or nurse can order a test for a patient with cold, influenza or COVID-19-like symptoms.
If you don’t have a doctor, you can call Island Health at 1-844-901-8442 to be assessed if you need testing. Appointments for COVID-19 testing must be pre-booked through a primary care provider or Island Health’s call centre.
Testing sites are unable to accommodate unscheduled or walk-in visits.
Island Health asks you to not go to a hospital emergency department seeking COVID-19 testing. However, if you have a medical emergency, you should call 911 or go to the nearest emergency department.
If you have questions for the NTC nurses, call Francine Gascoyne at 250-735-0416 or Catherine Gislason at 250-720-1763 from Monday to Friday 8 a.m. to 4:30 p.m.
“We will hear concerns then determine appropriate staff to address the concern. We still want people to be looking after their health,” said Gascoyne.