It has been more than a year since the first case of COVID-19 was identified in British Columbia. It started with a man living in the Vancouver Coastal Health Region who had just returned from Wuhan, China.
The man has since recovered but in the following months more than 69,716 cases of COVID-19 have been confirmed in British Columbia.
As of Feb. 5, 2021, a total of 1,246 British Columbians have died of COVID-19; at least three of those deaths were Nuu-chah-nulth people.
Leaders in the remote Nuu-chah-nulth communities responded early with strict rules designed to prevent outbreaks. Memories of another pandemic - and what it did to Indigenous populations on the west coast - are a stark reminder of what could happen.
In 1862 a miner sailed into Victoria, looking to strike it rich in the gold rush. He was the first person infected with smallpox on Vancouver Island. More came from San Francisco that year. Indigenous people had no immunity to smallpox or flu that was brought in by the foreigners.
Smallpox swept through coastal Indigenous communities like a wildfire, leaving death and destruction in its wake. In 1862, 17,000 Indigenous people, about half the population, died of smallpox on the west coast alone, according to University of Victoria research.
Today, as people race to save Indigenous language and culture, there is great concern that an outbreak of COVID-19 could have devastating consequences for the few elderly fluent speakers left. They are the most vulnerable population when it comes to surviving COVID-19.
Most Nuu-chah-nulth villages are remote. Some are only accessible by water and many are at the end of rough logging roads.
Cynthia Blackstone says Kyuquot, the most northern Nuu-chah-nulth community, has no road access.
“If there’s an emergency evacuation, it hast to be by helicopter and that is weather dependent,” said Blackstone, who is CAO of the Ka:'yu:'k't'h'/Che:k'tles7et'h' First Nations.
If there’s time and proper conditions, patients can be sent out by ambulance. But that means a half-hour boat trip in the best conditions – it could take longer if it’s dark or stormy. The patient would be handed over to paramedics who would take the rough logging road from Fair Harbour to Zeballos and finally to Port McNeill – a three-hour road trip.
Elmer Frank, Tla-o-qui-aht’s Emergency Operations Centre leader, notes that the Tofino General Hospital is not far from the Tla-o-qui-aht communities of Opitsaht on Meares Island as well as Esowista and Ty-histanis on Long Beach - but it’s not equipped to care for COVID-19 patients.
“We are in a state of emergency and our priority is to keep our elders and vulnerable people safe,” said Frank, adding that it would be catastrophic if the virus made its way through their communities. “We had two cases in our community so we closed it down. Residents and essential workers are the only ones entering and leaving the community.
Frank says that over the past year, 22 Tla-o-qui-aht members contracted the virus, both on and off reserve. Sadly, a Tla-o-qui-aht elder, one who lived in an urban centre, died after being infected.
In Tla-o-qui-aht’s case emergency patients would go to the West Coast General Hospital in Port Alberni, about two hours away by road. But there is a major construction site at Kennedy Lake that is sometimes closed and always adds to travel time.
Because of the isolation and lack of medical resources, many nations have closed their communities to outsiders in an effort to minimize contact with potential COVID-19 cases. Most nations have instituted a check-in system that allows them to track the comings and goings of their residents for the purposes of contact tracing and to minimize unnecessary trips outside the villages.
“We have a Pandemic Response Team and they review and respond to requests to leave the village,” said Blackstone.
In addition, members that don’t ordinarily live in Kyuquot are not allowed to enter.
“It’s essential travel only – medical, family emergencies and maybe shopping,” said Blackstone.
Elmer Frank points out that groceries are expensive in the tourist destination of Tofino and for that reason, the larger Tla-o-qui-aht families opt to go to a city for big grocery shopping trips. Designated household members are permitted to leave to get groceries and they check-in when they return home.
In Spring 2020 when the pandemic started, Blackstone said Kyuquot residents were more agreeable to lockdown conditions. But as time goes on people grow weary of the social isolation. And with the vaccine rolling out, people may feel emboldened to expand their social bubbles.
Provincial Health Officer Bonnie Henry warns that not enough people are vaccinated and it is not known if the inoculated can carry the virus to unvaccinated people. For those reasons, people are asked to remain vigilant and follow PHO orders.
But, like most communities, Kyuquot has a few people that are vocal about their displeasure with the pandemic rules.
“Some get denied (permission to leave the village) but most find a way out,” said Blackstone, adding that leadership remains concerned over the partying. “We have a problem with compliance; we still have people having parties and we’d like to find a way to have better enforcement.”
Over the past year the nation has allowed members to move back home under special circumstances.
“Say someone had a break-up, got kicked out and has nowhere to go,” said Blackstone.
If they have family to stay with in Kyuquot, they will be allowed home rather than be forced to live in the streets.
“We have had not one positive case in our community so we feel confident that the measures we put in place are working,” said Blackstone.
Frank reminds people to abide by the provincial health officer’s orders – no gathering, no visiting.
“We’ve seen how this virus moves and spreads. For now, it’s residents only at TFN territories,” he added. “Hopefully, one day soon, if we all keep still and bring the numbers down, we can get back to normal.”
On Feb. 2 the provincial government extended B.C.’s state of emergency.
“The state of emergency is extended through the end of the day on Feb. 16, 2021, to allow staff to take the necessary actions to keep British Columbians safe and manage immediate concerns and COVID-19 outbreaks,” stated the province.
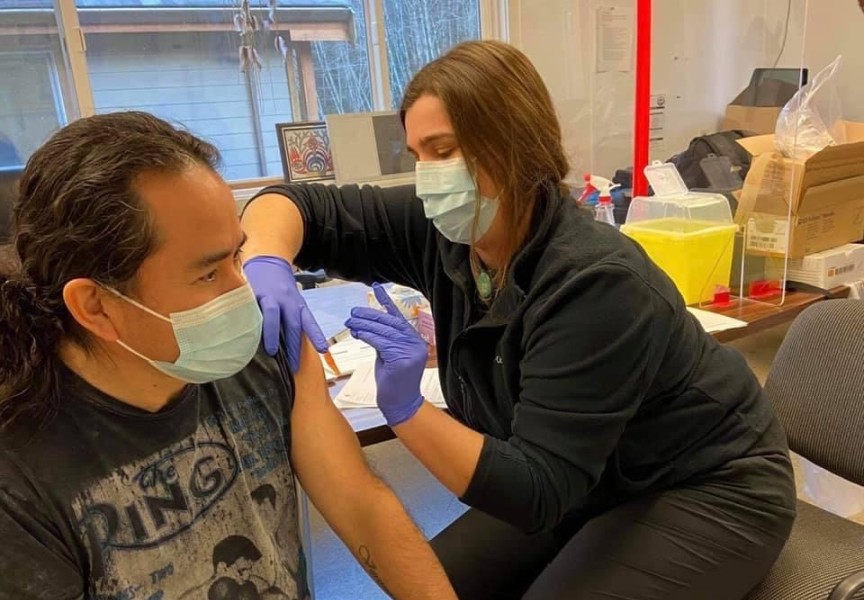
On Feb. 4 Dr. Evan Adams, chief medical officer at the First Nations Health Authority, reported that there were 172 COVID-19 deaths on reserves in B.C. over the past year. The good news is that since the vaccine began rolling out in late December, case numbers are dropping.
“Three hundred and ninety five First Nations communities out of 650 have had clusters,” Adams reported in a town hall information session.
There were more than 100 on-reserve new cases reported Feb. 3, but Adams said the provincial government has been committed to vaccinate Indigenous adults, and that he hopes this approach stays in place.
Nearly 150,000 vaccine doses were administered in B.C. as of Feb. 5, 2021.