Last year was the deadliest yet for fatal overdoses in B.C., and while many are calling for the decriminalization of street drugs, those with a close eye on the crisis are looking to medical professionals to take a larger role in prescribing safer alternatives.
For the better part of a decade deaths from illicit drug use rose in British Columbia - until progress with the public health crisis was evident when fatalities dropped by 64 per cent in 2019 to 984. But these positive gains reversed when the COVID-19 pandemic hit, resulting in 1,716 illicit drug deaths in 2020, a 74 per cent increase over the previous year.
There are now more deaths in B.C. due to illicit drug use than suicide, car crashes and homicide combined, and over 2020 overdose fatalities far exceeded the 901 attributed to COVID-19.
“One of the most insidious impacts of the pandemic has been increased toxicity due to disruption on the supply chain for illicit drugs across the country,” said Sheila Malcolmson, B.C.’s minister of Addictions and Mental Health, after last year’s fatal tally was announced by the B.C. Coroners Service on Feb. 11. “We stepped up our response to this emergency in B.C., but the illicit drug supply is dramatically more toxic than a year ago - and tragically, more lethal. Combined with the stigma that drives people to use alone and a pandemic that isolates them even further, you have a recipe for a terrible surge in overdose deaths.”
The overdose crisis has hit First Nations particularly hard. In 2019 First Nations people were almost four times more likely to die of a drug overdose than other B.C. residents. Statistics released from the First Nations Health Authority indicate that the pandemic made the situation more severe, as the fatality rate increased to 5.6 times higher than other people in B.C., based on data collected from January to May 2020.
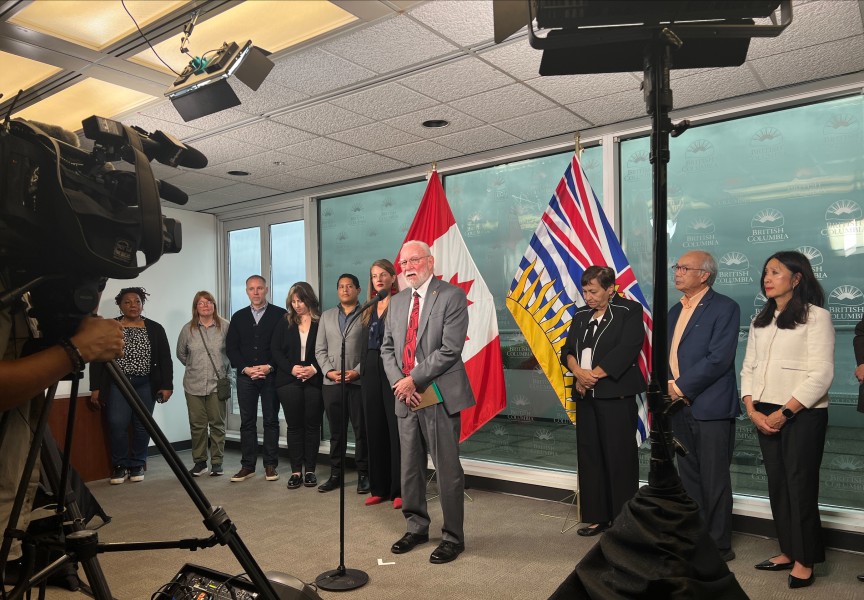
As she presented the latest numbers, Chief Coroner Lisa Lapointe emphasized the urgency for widespread change in how illicit drug use is handled in the province.
“What we’ve seen is decades and decades of treating problematic substance use disorder, addiction, as a criminal activity,” she said. “In many ways the policies that we have in place, have had in place for decades, have been a boon for illicit drug users and illicit drug suppliers because that’s where people have to go.”
During the coroner’s press conference Leslie McBain of the advocacy group Moms Stop the Harm noted that the public’s view of illicit drug users has hindered how governments and agencies responded to the overdose crisis.
“The response to COVID was coordinated, and it was strong,” she said. “The response to drug deaths by toxic supply has been sketchy, it has had huge gaps in it, it has not been attended to in the ways that it needs to be done.”
One proven means of preventing more deaths is offering supervised locations for drug users, as the coroner reported that not one fatality has been reported from these sites.
In Port Alberni use of the Overdose Prevention Site on Third Avenue dropped during the early weeks of the pandemic, but has since returned to high numbers, and hours of operation have even been extended to 8 a.m. to 8 p.m., seven days a week.
“Everybody thinks of an illicit drug user as somebody who is part of the marginalized people. That’s a fallacy,” said Wes Hewitt, executive director of the Port Alberni Shelter Society, which runs the OPS. “There’s a far greater number of people that use substances that are working people that have a house, have a career and a job, and are weekend users.”
To attend to the stigma of drug use and free up more police resources, Malcolmson spoke of working with the federal government to approve the decriminalization of illicit drugs. But police have already taken their focus away from drug possession, said Chief Constable Mike Serr of the Abbotsford Police Department during the coroner’s press conference.
“We are operating as if simple possession of illicit drugs is decriminalized,” he said. “The role of front-line policing has shifted to a harm-reduction approach.”
“The police aren’t prosecuting most average drug users, so I don’t really see that just decriminalization is going to make a great difference,” commented Hewitt. “What we need is a combination of decriminalization and a new approach, a better approach, to treatment in dealing with the individuals.”
Besides visits, referrals to treatment and opioid antagonist treatment has increased at the Port Alberni site in recent months. Lapointe stressed the role of medical professionals in diverting more users to safer, prescribed medications to shoulder their addictions. She wants physicians to immediately know what to do if a drug user comes to them with an addiction problem.
“What is the one thing that could stop those deaths? It is a safe, regulated, legal pharmaceutical supply of drugs that is available to people with substance use disorder,” added McBain.
Hewitt is seeing the system slowly change towards more prescriptions for pharmaceutical alternatives.
“Primarily we’ve got a couple of doctors, there’s other doctors that are starting to come on board,” he said.
But this is not necessarily an easy transition for physicians, cautioned Hewitt.
“They have to take training,” he noted. “For the average doctor, that’s just one more thing on his plate. Their practices are generally full, and they’re full with predominantly clients that don’t necessarily need that.”