An agency that provides substance use counselling to youth and families will be consulting with Nuu-chah-nulth First Nations to determine how to spend additional funds for overdose response.
West Coast Community Resources Society (WCCR) is among the 23 rural, remote and Indigenous communities and organizations to receive the extra support, totalling more than $1 million, from the B.C. Ministry of Mental Health and Addictions.
The funds — which amount to roughly $50,000 per group — are earmarked for helping small communities to expand local overdose response and awareness efforts through the ministry’s Community Action Initiative.
“We’re looking to provide the services that is most appropriate and needed, knowing that the last few months have been very, very challenging for a couple of communities on the coast,” said Margaret Morrison, executive director of WCCR.
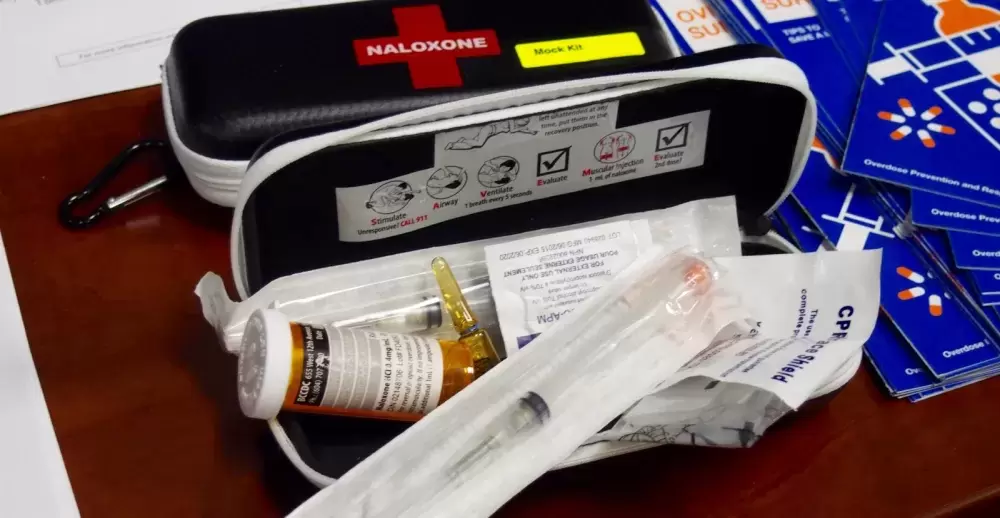
Morrison explained that the one-time grant will be directed pro-actively at overdose prevention and harm-reduction measures through education. That may involve provision of Naloxone kits, a potentially lifesaving medication for fentanyl overdose, training in administering Naloxone or instruction in the use of an app called Lifeguard, launched last year.
“It’s one way someone might minimize risk,” Morrison said.
Five years after a provincial health emergency was declared in an all-out response to illicit drug overdoses on an epidemic scale, the crisis continues to exact a deadly and ruinous toll.
More than 1,700 people died from fatal overdoses in B.C. in 2020. That amounts to above five OD deaths daily, and Indigenous populations are disproportionately affected. According to provincial data from January to October 2020, First Nations people died from overdose at a rate 5.5 times higher than other B.C. residents.
The second provincial health emergency — the global pandemic that continues to have First Nation communities in a state of high alert and in many cases closed to visitors — presents an added challenge in responding to the first. Fatal overdoses increased on central Vancouver Island over the past year, a trend that health officials believe has been worsened by the novel coronavirus pandemic.
“We want to respond to communities that are wanting to remain cautious,” Morrison said.
WCCS, which has offices in Tofino and Ucluelet, has one staff member currently dedicated to substance use counselling and may add another, she said. They may employ Zoom conferencing in order to provide services to communities temporarily closed due to pandemic concerns.
“But if that’s not going to answer a particular need by a community, we would hope to respond with whatever is most helpful,” she said.
People in rural and remote areas face major hurdles in accessing substance use services just as they do for health services in general. They often face longer travel distances to obtain health care and treatment. Access to the overdose antidote Naloxone and harm reduction services are sometimes limited in rural areas. Among Indigenous peoples, these factors can be compounded by a reluctance to access mainstream health services due to negative experiences in the past.
“Intergenerational trauma stemming from a history of colonization and racism has given way to a terrible reality that Indigenous peoples continue to be disproportionately impacted by the overdose crisis in the province,” said Murray Rankin, minister of Indigenous relations and reconciliation. “The crisis has only intensified during the COVID-19 pandemic. This new funding will help those struggling to connect with community-led, culturally appropriate programs, which is vital to recovery and promote healing.”
Morrison said she regrets that there was no chance to consult with First Nations in advance of their grant application in January. The deadline was “pretty tight” and it was evident as a result that other organizations were not responding in time, she noted. They were prepared to have their application rejected and would have welcomed another agency stepping up, she added.
In 2020, drug toxicity deaths increased by more than 50 per cent on the central Island, as numbers rose from 36 deaths in 2019 to 58 deaths in 2020. B.C. Coroners Service shows that there were 11 overdose fatalities in the Alberni-Clayoquot region in 2020.
Statistics tell only part of the overdose story, though. The broader reality is that most fatal overdoses occur within private homes when people are taking drugs alone. In many cases, they had people in their lives who may have been able to take preventive steps.
Morrison said there have been indications from neighbouring communities that the funding is necessary to ensure there is a response capability as needs arise.
“We have some knowledge of what might be helpful,” but will rely on community consultation to properly focus efforts, she stressed.