Indigenous people are dying from increasingly toxic illicit drugs at five times the rate of non-Indigenous people, a growing disparity that health officials blame on pandemic isolation, poor access to services and systemic racism.
B.C. was beginning to make progress against the overdose crisis after declaring a provincial health emergency in 2016. That was before COVID-19 struck.
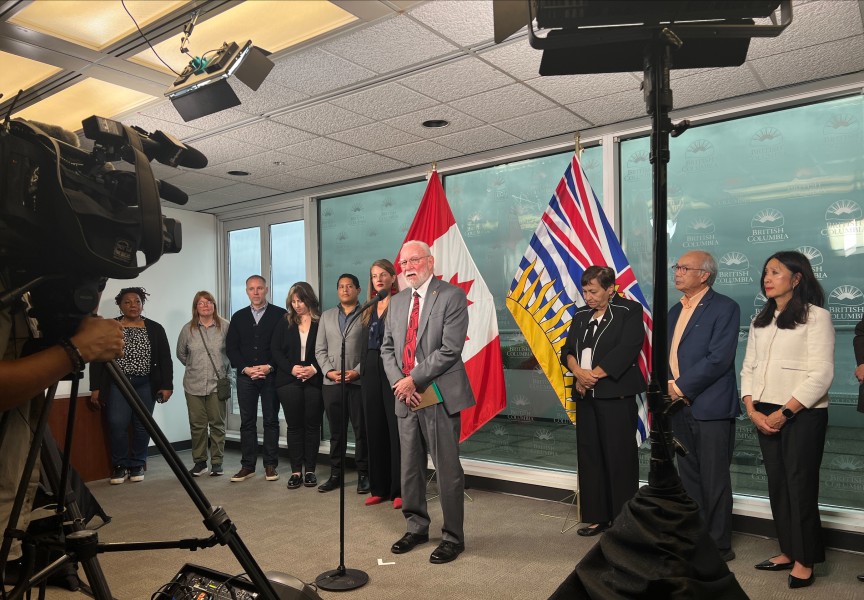
“Things have changed and not for the better,” said Dr. Nel Wieman of First Nations Health Authority in an online news conference May 27. “These dual crises have had significant impact on toxic drug overdoses and deaths overall.”
There were 1,716 overdose deaths in B.C. in 2020, a 74 percent increase over 2019. The deaths average out to 4.7 per day, two more than before the pandemic struck. While Indigenous people represent only 3.3 percent of the overall population, they account for about 15 percent of overdose deaths in the province.
Wieman said 254 Indigenous people died from toxic-drug overdoses last year, roughly a 120 percent increase over 2019.
“The rate at which First Nation people died has also increased,” Wieman said. “The gap is widening, and this is the widest gap we’ve seen since 2016.”
COVID forced people into isolation, leading to more addicts to use drugs alone, Wieman said. At the same time, it grew difficult if not impossible to access services during the pandemic shutdown. Public health measures intended to keep people safe had unintended consequences.
“We had been making some progress,” said Dr. Bonnie Henry, provincial health officer. “It’s shocking and horrifying to find that the conditions we put in place to manage the pandemic had exacerbated the overdose problem. We’ve also been seeing increased deaths among people isolated in their homes.”
“It is a crisis within a crisis and at times it feels overwhelming,” said Chief Coroner Lisa Lapointe.
Toxicity of the drug supply has increased during the pandemic due to closure of the Canada-U.S. border, disrupting the usual flow of illicit drugs. Henry said the situation makes it more urgent than ever to decriminalize small amounts of illicit drugs.
“We need to create a safe drug supply and make sure we have alternatives for people as the toxicity of the drug supply skyrockets,” said Dr. Bonnie Henry.
In March, the provincial government established a safe supply program that enables doctors and nurses to prescribe pharmaceutical alternatives to street drugs. The province is seeking federal government approval to become the first Canadian jurisdiction to decriminalize possession of small amounts of illicit drugs. Sheila Malcolmson, B.C. minister of mental health and addictions, has told Ottawa that the need for change is more urgent than ever due to the pandemic.
“This overwhelming loss of life is felt deeply in every community and we mourn with all the families, relatives, friends and caregivers that carry this loss,” Malcolmson said. “The collision of the pandemic, the poisoned drug supply and Indigenous-specific racism is at the root of the crisis we see today.”
“The messaging for the pandemic is that we’re all in this together, but this is not the case for the toxic drug crisis,” Wieman said. “We continue to lose more people in B.C. to the toxic drug crisis than to COVID-19, yet the issue is not receiving the attention it deserves. We need to change the narrative and work together to address the existing stigmas surrounding toxic drug use.”
First Nations have insufficient access to culturally safe health care as well as to addiction services, she said. On top of this, they experience intergenerational trauma, a legacy of residential schools.
While statistics don’t convey the full human impact of the crisis, the 2020 numbers point to disturbing trends. First Nations women, for example, died at 9.9 times the rate of other female B.C. residents. Men are most at risk, leading Island Health to launch an awareness campaign recently, encouraging men to break their silence about drug use.
Last year, 263 people died on the Island from overdose. Of that number, 225 were men, and 126 of them were in a private residence when they overdosed. Overall in B.C., half the men who have died from toxic drugs were employed. Of those, 55 percent worked in trades or transport.
“There’s no getting around it, 2020 was a devastating year,” Wieman said. “We need to build hope that we can turn things around and prevent more deaths.”
In response, FNHA launched an online substance use and psychiatry service, part of an initiative to create a range of accessible treatment and healing alternatives for people who use substances. The health authority has also supported expanded access to prescription alternatives and opioid agonist therapy. Education in harm reduction was expanded and online training sessions were added.
Lapointe said she is encouraged by agencies working in close collaboration, the passion of first responders and leadership in First Nations communities supporting clinicians in pursuing safer supply alternatives.
“I’m encouraged by people speaking out and demanding different approaches,” she added.
“The people in the communities are the first line in this crisis … so we are working very hard to support those people as well,” said Dr. Shannon McDonald of FNHA.
“We build hope by recognizing, just as with the COVID-19 pandemic, our way out of this crisis is by working together,” Wieman said.
The scourge has not let up in the last six months. There were 158 suspected illicit drug toxicity deaths in March 2021, according to the Coroners Service. This was a 41 percent increase over March 2020 and is tied with March 2018 for the largest number ever recorded in that month.
The Kuu-us Crisis Line is available for support at 1-800-588-8717.
Other resources available:
• Call the National Overdose Response Service before you use drugs to connect with people who want to help you stay safe. 1-888-688-NORS (6677). NORS is an overdose prevention hotline providing confidential, non-judgmental support.
• Download the LifeguardApp on your phone www.lifeguarddh.com
• Learn about safer use. Call B.C.’s Alcohol and Drug Information Referral Service 1-800-663-1441 or visit IslandHealth.ca/stopoverdose.