British Columbia is the first Canadian province to introduce a new policy that will expand access to a safer drug supply.
The Ministry of Mental Health and Addictions said that once the Prescribed Safer Supply initiative is fully implemented, people who use or are at risk of dying from drugs will have access to alternatives covered by Pharmacare. These will include a range of opioids and stimulants that will be determined by programs and prescribers.
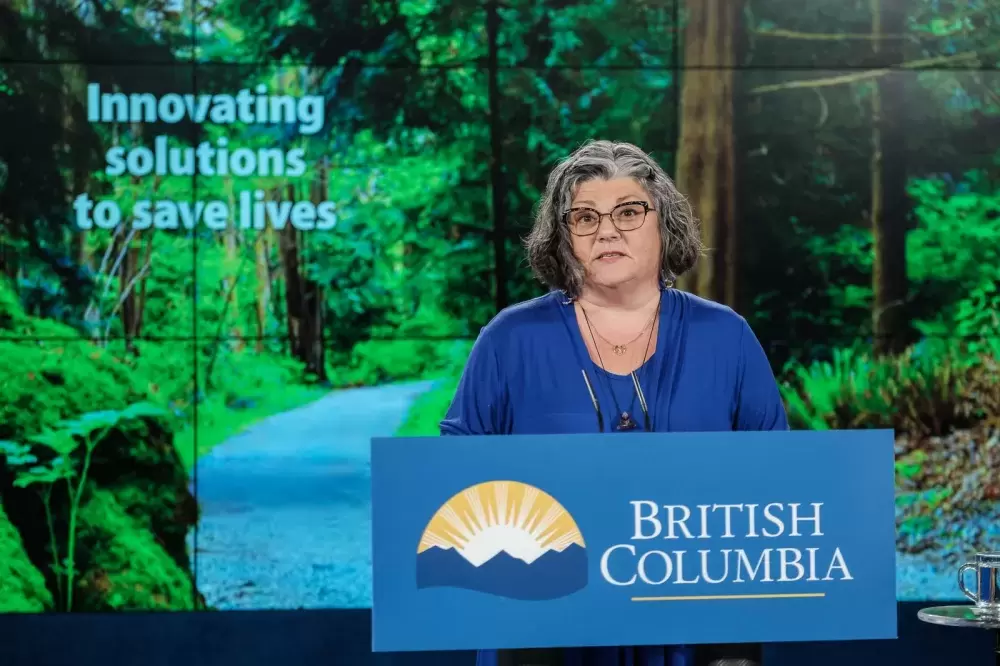
“With more than 7,000 lives lost to toxic illicit drugs, we need new measures to connect people to the supports they need to stay safe,” said Dr. Bonnie Henry, provincial health officer, in a release. “Reducing harm for people who use drugs is the right thing to do. Bringing in this new policy to expand prescribed safer supply is a big change for B.C.’s health-care system. It’s about meeting people where they are at, reducing risk of toxic drug death and connecting people to the care they need and deserve.”
The new policy was created in consultation with clinicians, people with lived experience, Indigenous partners, health authorities, among others, and will roll out in a phased approach.
The first phase will see the policy integrated into existing health-authority funded programs that prescribe drug alternatives. New programs, such as service hubs and outreach teams, will also be created to further provide prescribe safer supply services.
As data is collected, the first phase of the initiative is anticipated to remain in place for 18 to 24 months.
“Further phases will expand broader access once the clinical guidance is developed based on findings from the monitoring and evaluation process,” said the ministry.
For the next three years, the province will be directing $22.6 million in funding to health authorities to implement the program.
Dr. Shannon McDonald, First Nations Health Authority (FNHA) acting chief medical officer, said the initiative will provide “important tools to help reduce toxic drug overdose deaths among First Nations people who continue to be overrepresented as compared to the rest of the population.”
Based on racism experienced in the health care system, McDonald said there continues to be barriers for Indigenous peoples.
With 203 First Nations in B.C., and around 60 per cent of the First Nations population living away from home, Henry said that expanding access to more rural and remote communities is a “really important piece of this.”
McDonald said that this program will work in addition to harm reduction and treatment models, such as on-the-land treatment programs, that are already supported by the governments.
“We’re really looking at a holistic program of care that includes these medications, but there's also a broader range of services available to support people in community,” she said.
As the prescribed safer supply program develops, McDonald said there are details that still need to be worked out.
One of the main challenges will be the safe transportation of drugs to remote settings, she said.
Meanwhile, McDonald said that FNHA is working with nurses who operate in remote First Nations communities to help them become certified to prescribe opioid agonist therapies, a treatment for opioid addictions.
“The overdose crisis remains a public health emergency,” said Dr. Réka Gustafson, B.C.’s deputy provincial health officer, in a release. “During the pandemic, it was, by far, the most common cause of death in British Columbians aged 19 to 39. Response to a public health emergency requires us to use all available tools and to develop new ones to save lives. Safer supply is one of the suite of interventions that we have both the opportunity and the responsibility to implement as part of a co-ordinated and system-wide effort to end the overdose emergency in British Columbia.”
In 2020, there were 1,728 overdose deaths. It was the highest number of overdose deaths ever recorded. There have been 851 overdose deaths in 2021, compared to 569 in the same period of 2020.
According to the ministry, case studies have shown that access to a regular and safe supply of fentanyl patches improves connections with primary care services, reduces or eliminates illicit drug use, cuts down on the number of overdoses and hospitalizations, as well as improves social connection.
“We are certainly happy to have access to every tool in the available toolkit to respond to this ongoing [overdose] crisis,” said McDonald.