More than 2,200 people lost their lives to the toxic illicit drug supply in 2021, according to preliminary data from the BC Coroners Service.
Six more people die every day that decision-makers fail to respond to the crisis with “the urgency it demands,” British Columbia’s Chief Coroner Lisa LaPointe said.
“COVID-19 has shown what is possible when governments act decisively to save lives,” she said in a release. “And in order to save lives in this public-health emergency, we need to provide people with access to the substances they need, where and when they need them.”
Since being declared a public health emergency in April 2016, deaths due to the toxic illicit drug supply have increased by 400 per cent.
Last year saw the largest number of suspected illicit drug deaths ever recorded in British Columbia, with a 26 per cent increase in the number of deaths since 2020.
Drug toxicity is now only second to cancer for potential years of life lost in B.C.
“We cannot simply hope that things will improve,” said LaPointe. “It is long past time to end the chaos and devastation in our communities resulting from the flourishing illicit drug market.”
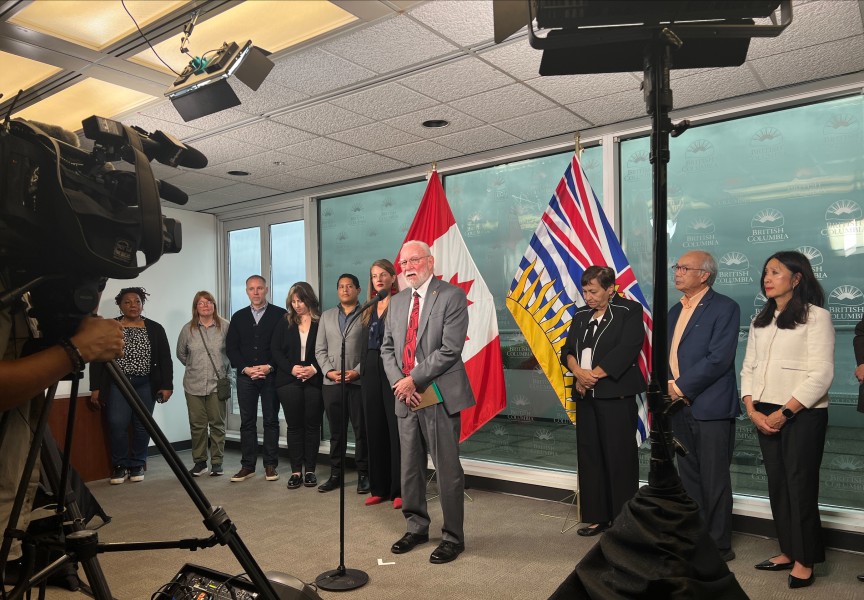
British Columbia is the first province in Canada to expand access to a prescribed safer drug supply. It is also the first to apply to the federal government to decriminalize the possession of small amounts of illicit drugs for personal use, asserting that “drug use is a healthcare issue and not a criminal justice issue,” Sheila Malcolmson, Minister of Mental Health and Addictions, said during a media briefing on Feb. 9.
“We are learning as we go,” she said. “We’re continuing to add new medications, for example – fentanyl patches can now be prescribed as a way to separate people from the toxic drug supply.”
Despite these moves, the BC Association of Social Workers is calling for the province to “redouble” their efforts in addressing the crisis.
Lapointe’s call for a massive increase in resources, and to ensure a safe, reliable, regulated drug supply is available “must be heeded,” said Michael Crawford, president of the BC Association of Social Workers.
In a joint-release, Provincial Health Officer Dr. Bonnie Henry and Malcolmson agreed that the number of deaths is “unacceptable.”
“We must reduce the fear and shame that leads so many to hide their drug use, avoid services and use deadly drugs alone,” the joint-release read. “Addiction is not a choice, it's a health condition.”
Over the past two years, Malcolmson said over 15,000 people have been prescribed a safe supply, and yet, “it’s not enough.”
“We’re determined to do more,” she said. “We all feel the urgency of this.”
The province will continue to make “systemic changes to our health-care system to build a comprehensive system of care for those experiencing substance use and mental health challenges,” said Malcolmson.
“The continued and terrible and unacceptable loss of life tells us that we need to do more,” she said.
Vancouver Coastal Health Peer Clinical Adviser Guy Felicella criticized the province’s approach, saying it “is killing and continues to kill people.”
“Every one of these deaths was preventable and represents a failure to act, a failure to learn from mistakes,” said Felicella. “Change nothing and nothing changes. That's been the story now for years as the approach throughout this crisis has been to meet policies where they're at, rather than meeting people who use drugs where they're at.”
Echoing Felicella, Nuu-chah-nulth Tribal Council (NTC) Vice-President Mariah Charleson said she hasn’t seen any “substantial” moves made by decision-makers and political leaders.
“It’s been over six years since B.C. has declared this a public health emergency,” she said. “You’d think there would be some type of urgency in response to this public health emergency, but we're not seeing the numbers decline.”
First Nations people have been disproportionately impacted by the toxic-drug poisoning. According to the First Nations Health Authority, First Nations people died at 5.3 times the rate of other B.C. residents in 2020.
While Charleson said a safe drug supply is critical, “the reality is there’s really few people who are actually benefiting from the few programs that are operating.”
People living in rural Nuu-chah-nulth communities “definitely don’t have access to safe supply,” she said.
In its final report, the Truth and Reconciliation Commission made 94 Calls to Action to address the legacy of residential schools. Similarly, the In Plain Sight summary report made 24 recommendations to eliminate Indigenous-specific racism within B.C.’s health care system.
“We need to really look at these documents and start responding,” said Charleson. “We know that trauma is the root cause for a lot of this self-medication. We know that the Indian Residential School System has had lasting effects. We’re all still affected. And that trauma is real – it’s still living within each and every one of us.”
The provincial and federal governments need to respond to these calls to action with “urgency,” she said.
“We really need to begin to look at prevention from the day a child is born,” she said. “We need to meet people where they're at. We need to be on the ground. We need to have the same amount of resources and money available that we've seen in response to other big, urgent crises such as COVID-19.”
Malcolmson said the province is now spending $2.7 billion every year “to respond to the overdose crisis and to attend to people’s mental health.”
“Fighting COVID-19 on the foundation of an intact healthcare system is very different from fighting the overdose public health emergency, while building a system of care at the same time,” she said.
But as every health authority in B.C. experienced a record loss of lives last year, LaPointe said enough is enough.
“Time has run out for research and discussion,” she said. “It is time to take action."