January 31 marked the one-year anniversary for B.C.’s three-year decriminalization pilot project, where people using up to 2.5 grams of certain illicit drugs would not face seizures, charges, or arrests. But as 2023 saw a five per cent increase in death rates, experts are pushing for expanding the prescribed safer supply to help users on their recovery journey.
“When we're looking at overdose deaths… one of the things we know very clearly is that people are dying because there's an extremely toxic supply of drugs,” said Kora DeBeck, an associate professor at Simon Fraser University’s School of Public Policy.
With no health or safety regulations in place, shared DeBeck, the drugs that people have access to are produced by drug cartels and organized crime.
“People do not know what they're taking,” she said. “We know from toxicology reports and monitoring the overdose deaths that the drug supply is getting more toxic and that is due to how drugs are being produced.”
In 2023, deaths due to unregulated and toxic drugs reached a high of 2,511 people in British Columbia, averaging 6.9 deaths per day, the largest number reported in one year.
With unregulated and toxic drugs as the leading cause of death for those aged 10 through to 59 in the province, the B.C. coroner confirms that “illicit fentanyl continues to drive the toxic drug crisis.”
“Fentanyl and its analogues were by far the most regularly detected substances, appearing in more than 85 per cent of test results conducted in 2023,” reads the coroner’s report on last year’s results.
While B.C.’s overdose death rate increased by five per cent since 2022, provinces that have not implemented decriminalization and harm reduction efforts as much as B.C. have seen an even steeper increase in fatalities, said Courtenay-Alberni MP Gord Johns.
“We have the lowest increase of the four major provinces with the highest death rate in the country,” said Johns. “We need to be going the other direction and if we treat this like a health emergency and we filled those gaps, we would see those numbers drop significantly.”
“[It’s] unequivocally clear and unanimous in that criminalizing people who use substances causes more harm, especially when people are using toxic, unregulated street drugs that are poisoned,” continued Johns, adding that upper levels of government need to move faster. “There's a lack of coordination, a lack of integration to fill those gaps, and a lack of will to see this as the crisis that it is.”
Johns stresses that the overdose crisis needs a more available safer supply of substances, “treatment on demand,” more stabilization beds and detox facilities that are accessible to people in their communities.
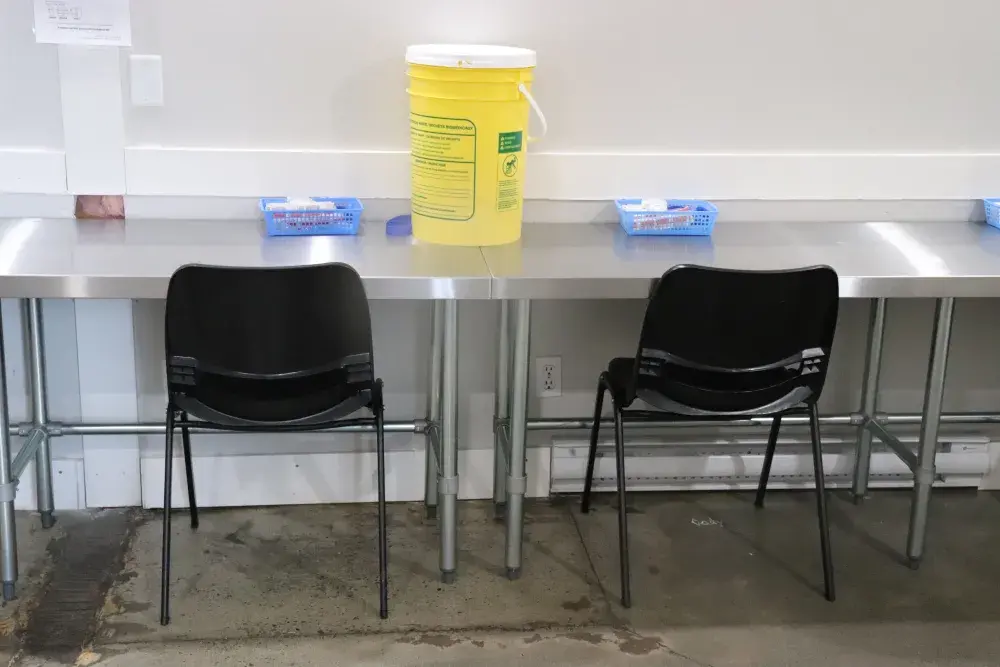
Since 2020, when the federal government first launched the safer supply pilot project, people have been able to access prescribed alternatives at a total of 10 locations, but DeBeck shared that these projects are on a small scale.
Of the estimated 115,000 people in the province who have opioid-use disorder, 4,331, less than four per cent, have accessed the province's prescribed safer supply program, said Alexis Crabtree, senior scientist and medical lead of harm reduction and substance use at the B.C. Centre for Disease Control.
One of the most significant limitations of the current model of prescribed safe supply is that hydromorphone, an opiate often prescribed, does not match up to the strength of fentanyl, said DeBeck.
“People who are dependent on fentanyl, if they're prescribed hydromorphone… generally they can't really even get enough in their system to avoid withdrawal,” she said, noting that this has been an “inadequate implementation” of something that could be promising.
“We know from research, really across the spectrum, that it's been very small the number of people who’ve been able to access it and the implementation of it has not been ideal,” said DeBeck.
But a recently published report from Provincial Health Officer Bonny Henry recommends an expansion of prescribed substances that are available to meet the needs of people who use drugs, including heroin, fentanyl, and stimulants.
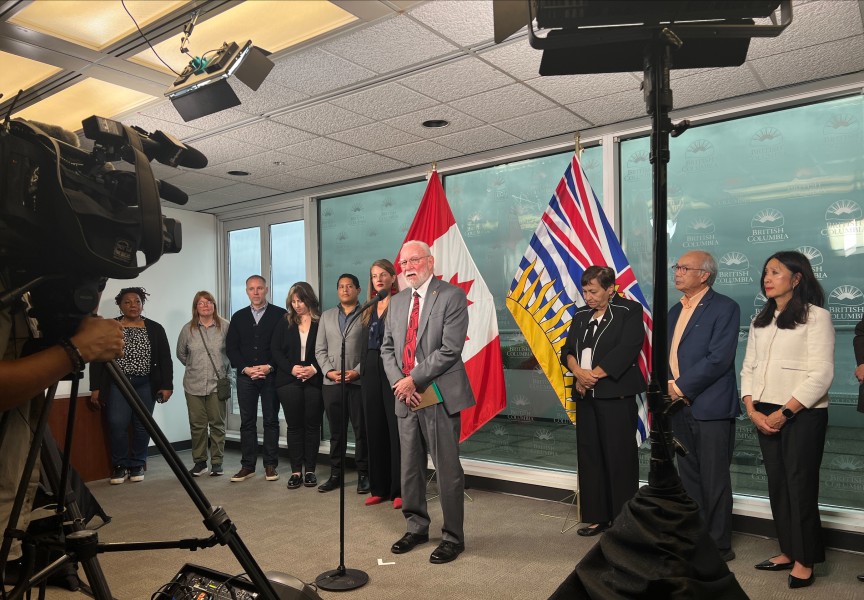
“This policy, in its intent, is an important part of the spectrum of medical care that we are providing and that we need to continue to provide for people who use drugs in this province,” said Henry at press conference for the report's release. “The program as it is right now does not go far enough in terms of the medical model to meet those needs or provide that degree of care that we need.”
Prescribed safer supply can help reduce the rate of drug poisoning events, connect people to wrap-around services and decrease reliance on unregulated drugs, said Crabtree.
“If people have access to a regulated supply of drugs, so that is… they have a known quantity and known purity of drugs, they are less likely to die of a fatal overdose,” said DeBeck.
“When we talk with people who use drugs, or who have used drugs, the term recovery means something very different for many of them,” said Henry. “It’s not a medical term, but it’s about being able to live in safe housing, to care for their family, to have meaningful employment, regardless of the use of… prescribed safer supply or use of [opioid agonist treatment].”
But Henry also notes that throughout the medical community, the term ‘recovery’ and its affiliation with abstinence, needs to shift.
“Many in the recovery communities also equate recovery with abstinence and many homes, for example, won’t accept people even on therapy like [opioid agonist therapy],” said Henry.
“It's certainly not surprising to see that overdose deaths are as high as they are, because we have not meaningfully addressed the production and the supply of drugs,” said DeBeck.