With the toxic drug crisis as the leading cause of death for British Columbians aged 10 though 59, nearly 170 youth, aged 18 and under, have lost their lives since 2017. According to experts, not enough research and monitoring has been done to assess the impacts of the crisis on young people, who also face barriers when accessing harm reduction services.
“Young people do use drugs,” said Kora DeBeck, an associate professor at Simon Fraser University’s School of Public Policy, noting that for young people it is a time of experimentation. “Unfortunately, in this context of a toxic drug supply, use can be so much more risky than it was 10 years ago.”
Between Jan. 1, 2017 and Dec. 31, 2022, the province saw 142 deaths from illicit drugs among minors, equal to 24 fatalities per year, according to a report released by the BC Coroners Service. With unregulated and toxic drugs as the leading cause of death, fentanyl or its analogues were detected in 78 per cent of the cases.
The next age group cited in the report, 19-29, saw more than 10 times the number of fatalities due to illicit drug use with 1,718 over the same period, and the 30-39 bracket had even more deaths at 2,580.
Of the youth, 73 per cent were recipients of one or more services from the Ministry of Children and Family development, while 67 per cent had either a diagnosis or evidence of a mental health disorder, the report continued.
According to coroner, deaths in 2023 due to unregulated drugs decreased among youth.
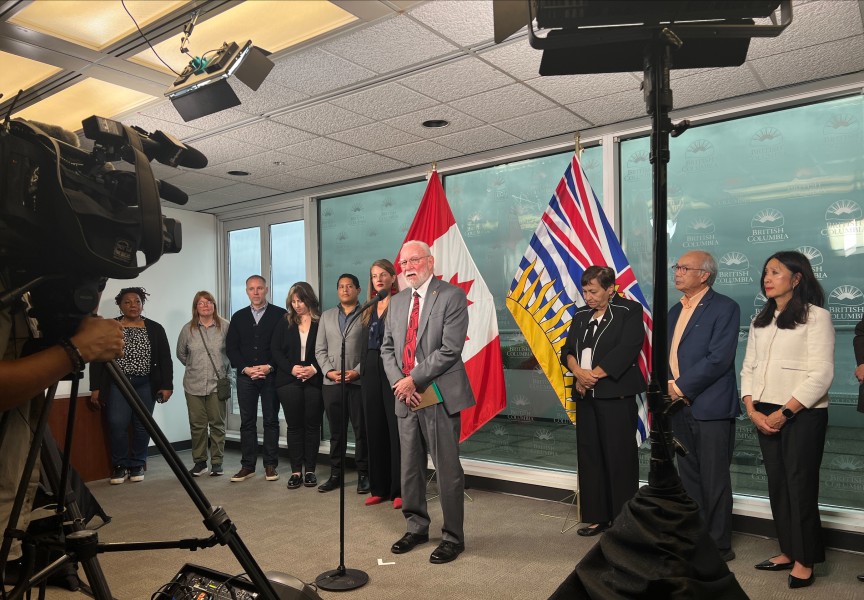
Data collected until late 2022 demonstrates that there has been no increase in the rate of youth being diagnosed with opioid use disorder since 2020, shared Alexis Crabtree, a senior scientist and medical lead of harm reduction and substance use at the B.C. Centre for Disease Control, at a recent press conference.
“Clearly though, more monitoring is needed,” said Crabtree. “The truth is, we don’t have a lot of evidence about what is happening for youth and substance use.”
“There is a need for more primary data collection with youth to understand what their experience of substance use is right now, and how the pandemic has shaped that, and what supports they might need in the future,” Crabtree continued.
DeBeck is the principal investigator for the At-Risk Youth Study (ATYS), which since 2005 has studied over a 1,000 street-involved youth under the age of 25 who use drugs in Vancouver. She said that based on feedback from the community there is frustration among young people from the barriers they face when accessing services.
“For young people, [they] often don’t have access to harm reduction services to the extent that older people have,” said DeBeck. “A lot of it is a reluctance to give them access to evidence-based harm reduction programs, I think out of fear that they might encourage substance use among young people or somehow send the wrong message.”
“The impact is that young people aren't given the protections that those evidence-based interventions can provide,” added DeBeck.
Because of this, young people who inject drugs are more likely to share needles, said DeBeck. But she noted that barriers for young people who use drugs extend much farther into housing, addiction treatment, food, nutrition, dental care and decriminalization.
“They're already using drugs, and they're already at risk,” said DeBeck. “There's a feeling that they're just not able to benefit from the protections that older people do get.”
In early February the Provincial Health Officer Bonnie Henry released a report recommending that the province expand its prescribed safer supply program to include heroin, fentanyl and stimulants to meet the needs of drug users. But concerns were raised among physicians about prescribing drugs to youth, Crabtree noted at the press conference.
“What they’re worried about is youth accessing these medications and transitioning to other forms of substance use,” said Crabtree.
DeBeck shared that with scaling up the prescribed safer supply, pharmaceutical drugs could, at a community level, “be more easily available, lower cost, and potentially even [be] perceived as being lower risk.”
“In that context, there could be young people, or people across the spectrum, who wouldn't otherwise use drugs, who might then feel like the risks around using drugs are lessened,” said DeBeck.
But with physician concerns, DeBeck believes that the situation should be monitored.
“I haven't seen any hard evidence that there is sort of a new epidemic of opiate use among young people that has been spurred on by diversion,” she added.
But another aspect of diversion could have benefits, shared DeBeck.
“If diversion becomes a substitution for other individuals away from unregulated street drugs, yes, that is a good thing,” she said.
Kali Sedgemore of Namgis First Nation, who works in Vancouver with youth who have lost a parent to the toxic drug crisis and now use drugs, shared that though diversion does occur, it’s not common for youth.
“[Youth are] finding what they want to get, which is usually fentanyl because they’re already… addicted to it,” said Sedgemore.
DeBeck shared that for prescribed safer supply programs, it’s important to consider if people can access the drugs they need and prefer.
“If there's a mismatch between what's offered and what people need, then we are going to increase the issues of diversion,” said DeBeck, who notes that, to date, the implementation of prescribed safer supply programs have been limited in the scope and types of medications provided.
The prescribed safer supply, with its limits around medications, “has created a lot more diversion and potential negative impacts than would be if we had a more to scale, rigorous, safe supply program,” said DeBeck.
For youth in Vancouver, Sedgemore shared that there needs to be a detox center and overdose prevention site dedicated to them.
“The reality is that youth are using drugs,” said Sedgemore. “By not teaching them harm reduction education and best practices, it’s putting them more in harm's way because it’s just teaching youth that their life’s not worthy.”